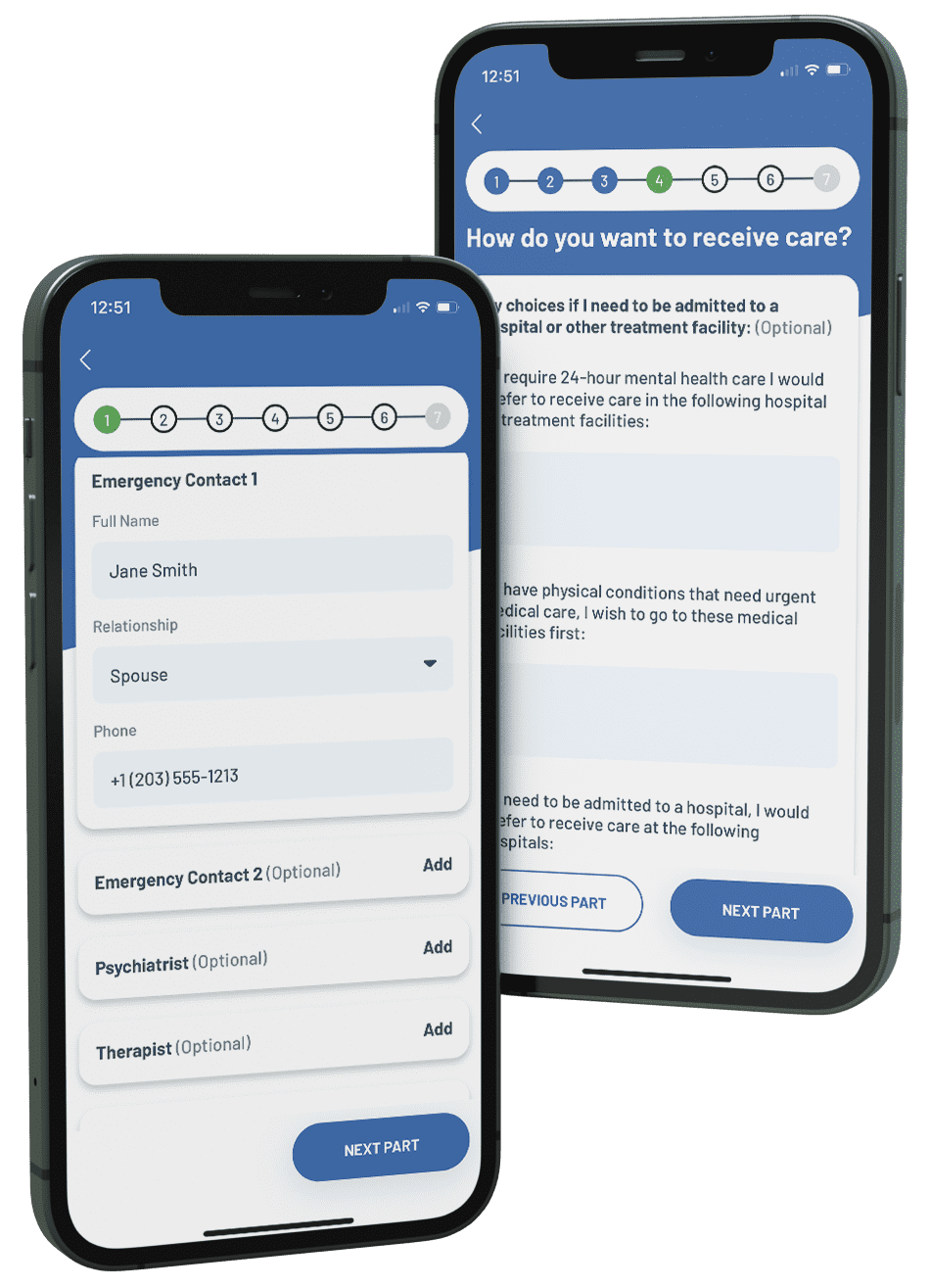
A PAD or psychiatric advance directive is a written document that has two parts. The first part is called an ‘instructional directive.’ It is a list of instructions and information that you wish to be followed if in a mental health crisis. For example, you might request admission to a certain hospital or refuse admission to another.
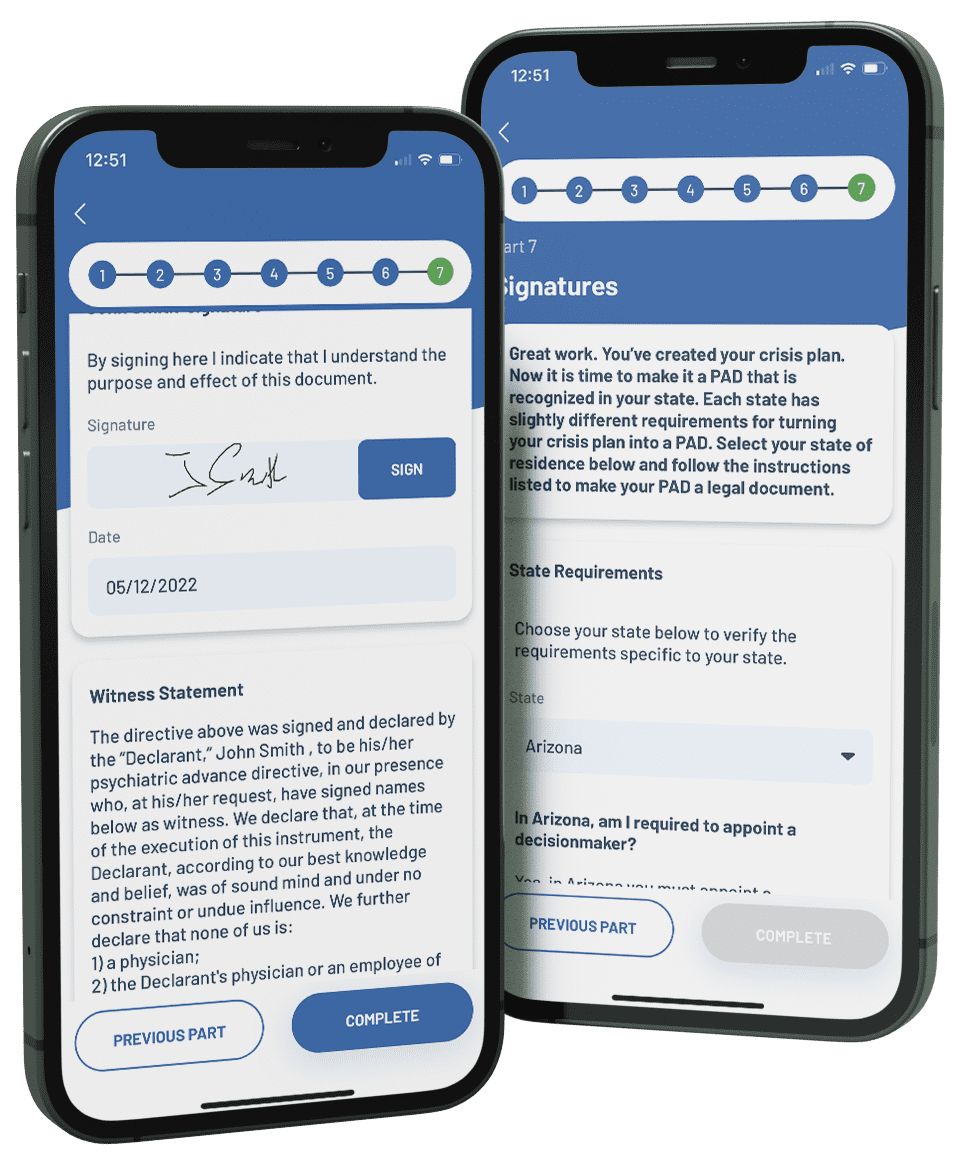
The second part of a PAD is a choice of a trusted person to make decisions for you if you are in crisis. In certain states, you must appoint a decisionmaker to carry out the instructions in your PAD. These states are: AZ, AR, CO, GA, IN, IA, KS, MA, MI, MS, MO, NE, NV, NH, RI, SD, UT, WI. If you do not live in one of these states, you may choose to have both parts or only one part.
You may also choose substitutes if the person chosen to make decisions is unavailable. The person chosen to make decisions may have different titles in different states. For now, we will call that person the ‘decisionmaker.’
A PAD is official once it has been signed by witnesses in from of a notary public and given to the patient’s doctors, providers and hospitals.
In a PAD, you may choose a trusted person to make decisions for you if you are in crisis. You may also choose substitutes if the person chosen to make decisions is unavailable. The person chosen to make decisions may have different titles in different states. They may be called a ‘Healthcare Agent’ or ‘Proxy’ or ‘Healthcare Power of Attorney.’ For this guide, we will call that person the ‘decisionmaker.’
The decisionmaker is notified when you are in crisis. The treatment team will then review any treatment decisions with the decisionmaker. The decisionmaker may approve or consent to any decisions that you could make if you were well. The decisionmaker makes decisions based on what he or she knows about your wishes. These wishes might come from the PAD or your discussions with your decisionmaker.
You should choose someone that you know well and trust to be your decisionmaker. The decisionmaker should review the PAD and agree to follow it. The decisionmaker can be a relative or friend but cannot be your doctor or treatment provider. If possible, you should choose at least one back up decisionmaker in case your first choice is unavailable during a crisis.
A PAD is an opportunity to try to make your mental health treatment in the future be the best it can be. You should think about past treatment. What has gone well? What has not gone so well? What might I want to change? What do I want providers to know if I cannot speak for myself? Which doctors should be contacted? Which family members or friends should be contacted? To which hospital do I wish to be admitted? Which medications might I want to take? Which would I not want to take? Who do I trust and knows me well enough to be my decisionmaker?
Click here to watch a video and learn about your medication choices
Click here to watch a video and learn about your hospital choices
Once a PAD is completed and signed by you and your witnesses, it is ready to be used in a crisis. Some states require you to get the PAD notarized. The PAD then goes into effect when a doctor you and feels that you cannot make or communicate treatment decisions. That means you are found to ‘lack capacity’ and the doctor writes that in your medical record. The PAD is then in effect until the doctor feels that you can make decisions again. The treatment team then is required to read the PAD and call in the decisionmaker to help make decisions. The treatment team is required to make every effort to follow the instructions in your PAD and those of the decisionmaker whenever possible.
The legal term for an inability to make healthcare decisions is called ‘incapacity.’ This means a doctor has examined you and found you are unable to make or communicate decisions about treatment. This must be written in the medical record by the doctor who examined you. The doctor must also determine when you are well again and has regained capacity and are again able to make your own decisions about treatment. That will also be written in the medical record. If it appears that you will be unable to make treatment decisions for a longer period of time, a court may find the patient is ‘incompetent’ and appoint a guardian.
A PAD is followed when a doctor who has examined you feels that you cannot make or communicate treatment decisions. That means you are found to ‘lack capacity’ and the doctor writes that in your medical record. The PAD then goes into effect. Most states recognize that there are situations in which some or all of the PAD cannot be followed. Even if one part of a PAD cannot be followed, the rest remains in effect and providers should follow it.
In general, a PAD may not be followed if a part is not feasible. For example, if you ask to be admitted to a hospital that is full, the treatment team may try another hospital. A PAD may not be followed if the treatment team thinks the request is not good medical care. For example, if you request a medicine that could be harmful, the request may not be followed. If you are under involuntary commitment or another emergency law, the PAD might not be followed.
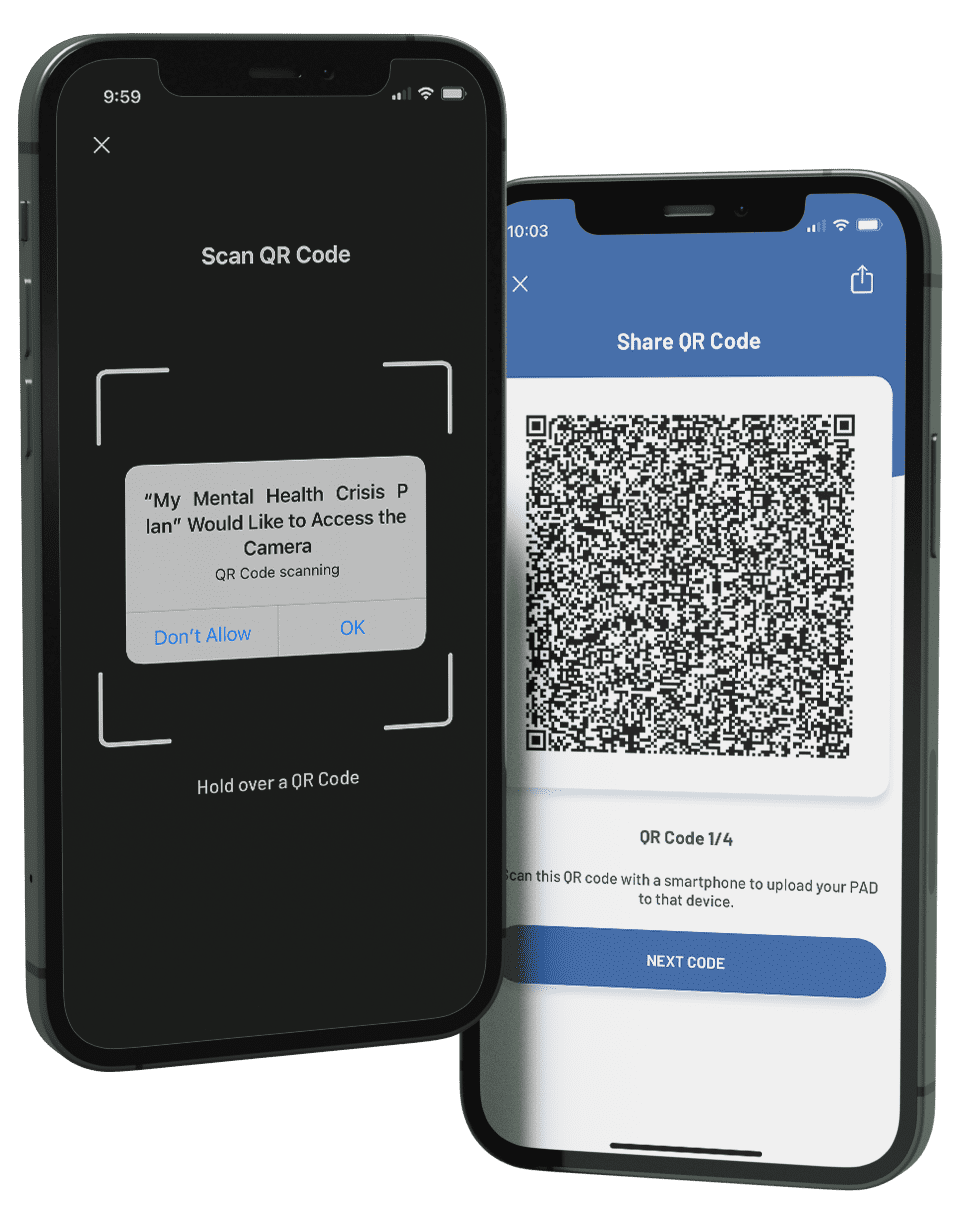
Once a PAD has been completed, it must be signed by two witnesses, sometimes in front of a notary public. This app will provide instructions specific to your state after you create your PAD. Your PAD is then ‘official’ and can be put into your medical record wherever you wish. That includes an electronic medical record where it can be read by providers taking care of you. There are also websites in some states where PADs can be stored for use in a crisis. It should be given to all of your treatment providers and your decisionmaker, if you have appointed one. This app allows you to create a PDF of your official PAD, store it in the app for easy access, and share it with whomever you choose.
A PAD maybe changed any time you wish, as long as you have ‘capacity’ (able to make or communicate treatment decisions) and is not in a mental health crisis. In most states, a PAD cannot be changed when you ‘lacks capacity’ and is in crisis. However, when are well again, you can re-do the PAD with new information or choices and have the new PAD witnessed and notarized. You may also change the decisionmaker in this process, if you have appointed one. When you are well, you may also decide that you no longer want a PAD altogether and declare that by telling that to treatment providers or putting that information in your medical record.